For questions/concerns about this disease in humans, please call your doctor or the Montana Department of Public Health and Human Services (DPHHS).
For questions about this disease/parasite in wildlife, please call the FWP Wildlife Health Lab at 406-577-7882.
Tularemia is a disease of both animals and humans caused by the bacterium Francisella tularensis. Rabbits, hares, and rodents are very susceptible, and often die in large numbers in an outbreak of the disease (CDC).
Geographically, tularemia has been reported in Canada, Mexico, and the United States (all states except Hawaii). With the exception of the Iberian Peninsula, tularemia is distributed throughout Europe and Mediterranean Africa, and has been identified in China, Iran, Israel, Japan, Korea, Russia, and Turkey (AVMA). Tularemia is widely distributed in the Northern Hemisphere (Adrian, 1981). Since its identification, the disease has been reported in all of the continental U.S. (Michigan, 2010).
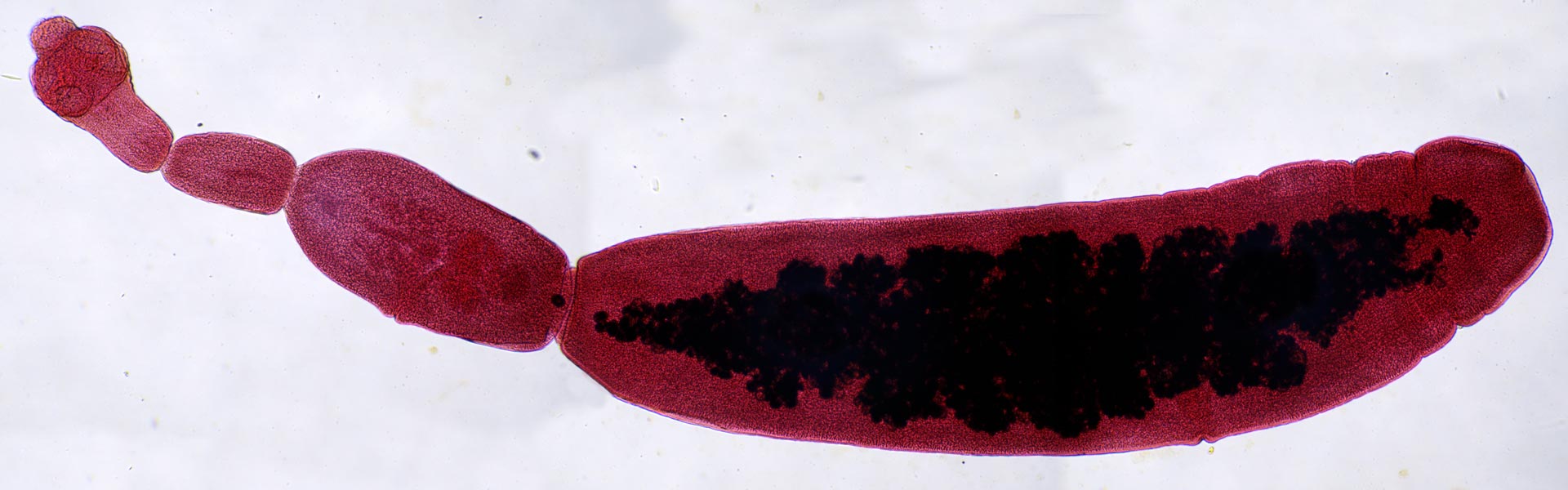
Tularemia most commonly infects hares, rabbits, and rodents such as prairie dogs, ground squirrels, beaver, and muskrat (Stitt, 2011); however, many species of mammals (including humans), birds and possibly even reptiles can be infected. Opossum, shrew, weasel, fox, coyote, dog, bobcat, cat, sheep, mule deer, white-tailed deer, and man have been infected (Adrian, 1981).
Tularemia can be transmitted to animals and humans by arthropods (mites, ticks, flies, midges, black flies, fleas, mosquitoes and lice), by contact with infected vertebrates, and by inhalation of feces-contaminated dust or ingestion of insufficiently cooked infected carcasses. In addition, waterborne epidemics have been reported, and F. tularensis has been found in ponds where there were epidemics among beavers in the northwestern U.S. Water may remain infectious for weeks to months following contamination (Miller et al, 2003).
Any infected animal can serve as a source of infection for humans, however, human infections are usually the result of dressing or skinning infected rabbits. In the U.S., rabbits are the source of infection in 90% of human cases (Michigan DNR).
Symptoms of tularemia are not always evident in wildlife due to the short duration of infection before death occurs. Most infected wild animals are found moribund or dead (Michigan, 2010; Adrian, 1981).
Infected hares and cottontails have been observed to behave oddly, run slowly, and be captured easily. Infected rabbits appear to be tame or in a stupor; they do not raise their heads or carry their front feet well. They rub their noses and forefeet into the ground, have recurrent muscle spasms, and stagger for a few yards between spasms. Clinical signs in experimentally infected red foxes included loss of appetite, diarrhea, and noisy, labored breathing (Michigan, 2010).
Symptoms of tularemia in humans vary depending on how the bacteria enters the body, and disease ranges from mild to fatal. Tularemia in humans always presents with fever (CDC). The following list taken from the CDC website describes the most common forms of Tularemia in humans.
Human infections result from the bite of arthropod vectors (ticks, deerflies, and occasionally mosquitoes) which are either infected or have contaminated mouthparts, direct contact with infected tissues or carcasses, ingestion or inhalation of soil or water contaminated by excreta or carcasses of infected animals, or inhalation of dust from pelts and paws (Miller et al, 2003; Stitt, 2011). Most human infections are the result of dressing or skinning infected rabbits. In the U.S., rabbits are the source of infection in 90% of human cases (Michigan, 2010).
To prevent exposure and infection with Tularemia during outdoor activity, use insect repellents and wear long pants, sleeves and socks to keep ticks and flies off your skin. Always remove attached ticks promptly, and don’t drink untreated surface water.
To prevent exposure while doing yard work, avoid mowing over sick or dead animals.
If you hunt or trap, use gloves when handling animals or carcasses, especially rabbits, muskrats, prairie dogs and other rodents. Always cook game meat thoroughly before eating.
All game meat should be cooked thoroughly to a temperature of at least 165° F (Stitt, 2011). If you harvest an animal and are unsure whether it is safe to eat, contact your local FWP staff for guidance soon after the animal is harvested.
Adrian, W.J., editor. 1981. Manual of Common Wildlife Diseases in Colorado. Denver: Colorado Division of Wildlife.
American Veterinary Medical Association. AVMA. Tularemia Facts. Website. https://www.avma.org/tularemia-facts#distribution
Michigan Wildlife Disease Manual. 2010. Michigan Department of Natural Resources. Website
Miller, M.J.R., R.D. Dawson, and H. Schwantje. 2003. Manual of Common Diseases and Parasites of Wildlife in Northern British Columbia. University of Northern British Columbia.
Stitt, Tyler. 2011. Diseases You Can Get From Wildlife - A Field-guide for Hunters, Trappers, Anglers and Biologists. British Columbia Ministry of the Environment.
